The Vagus Nerve + Your Meds: Why "Body Stuff" Matters in Psychiatry
- Antoinette Goosby
- 12 minutes ago
- 5 min read
You know that feeling when your therapist says "just breathe" and you kind of want to roll your eyes? Or when someone suggests yoga for your anxiety and you're thinking, "I'm literally on Zoloft, how is downward dog going to help?"
Here's the thing: they're not wrong. And your medication isn't failing you. The truth is, your brain and body aren't separate systems, and treating them like they are might be why you're still feeling stuck.
Let me explain.
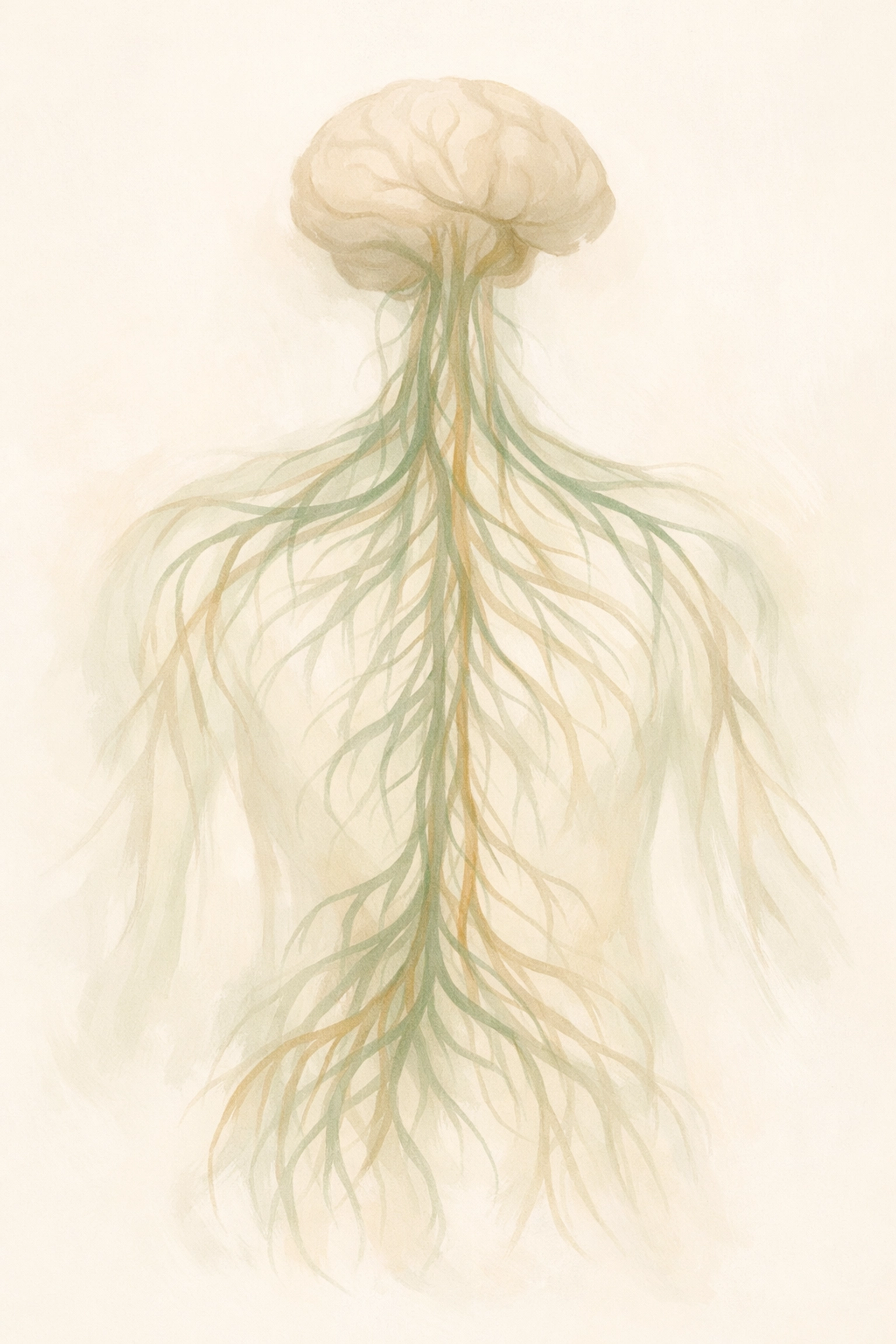
Your Body's Secret Superhighway
The vagus nerve is basically the longest nerve in your body, running from your brainstem all the way down to your gut (and hitting your heart, lungs, and a bunch of other organs along the way). Think of it as the main communication highway between your brain and everything else.
When someone talks about being "in their body" or "grounded," they're really talking about this nerve doing its job well. The vagus nerve is your parasympathetic nervous system's MVP, it's what tells your body to chill out after stress, regulates your heart rate, helps you digest food, and even influences how you connect with other people.
Here's where it gets interesting for psychiatric care: vagal tone, basically how strong and flexible this nerve is, directly impacts your ability to regulate emotions and recover from stress. Low vagal tone? You might find yourself stuck in fight-or-flight mode, struggling to calm down even when the stressor is gone.
Why Your Medication Needs a Dance Partner
As a student dance movement therapist and psychiatric nurse practitioner, I see this all the time: someone comes in on a solid medication regimen, maybe an SSRI for depression or anxiety, and they're like, "It's helping, but I still feel off."
That's not failure. That's your body asking for the other half of the equation.
Here's the science part (I'll keep it quick): Psychiatric medications work on neurotransmitters like serotonin and norepinephrine. Guess what else affects those same neurotransmitters? Your vagus nerve. In fact, research shows that vagus nerve stimulation enhances norepinephrine activity in the same brain regions that antidepressants target.
So when you take your medication but you're also:
Sitting hunched over a laptop for 8 hours
Holding your breath through stressful moments
Never moving your body
Ignoring signals like hunger, fatigue, or tension
...you're basically asking your meds to do all the heavy lifting while your body's natural regulation system is offline.
The Inflammation Connection
Here's something they don't always tell you: depression and anxiety aren't just "chemical imbalances" in your brain. They're often connected to inflammation in your body. Low vagal tone is linked to increased inflammatory markers, which, surprise, makes depression worse.
Your vagus nerve actually has what's called a "cholinergic anti-inflammatory reflex." Basically, when it's working well, it tells your body to chill out on the inflammation. When it's not? Your body stays in a low-grade inflammatory state that no amount of Lexapro can fully fix on its own.
This is why holistic psychiatry isn't just a buzzword. It's recognizing that your gut health, your sleep, your breathing patterns, and your movement (or lack thereof) are all part of your mental health picture.

What "Body Stuff" Actually Looks Like
Okay, so what does this mean in practice? I'm not asking you to become a yogi or run marathons (unless you want to). Somatic strategies, fancy term for body-based work, can be really simple.
Deep, Slow Breathing When you breathe slowly (like, 4-6 breaths per minute instead of the usual 12-20), you're directly stimulating vagal afferent fibers. This isn't woo-woo, it's measurable. Slow breathing increases vagal tone, which improves your ability to regulate emotions and recover from stress.
Try this: Breathe in for 4 counts, hold for 4, breathe out for 6. Do it for two minutes. That longer exhale activates your parasympathetic nervous system, the rest-and-digest mode.
Gentle Movement This is where my dance movement therapy background comes in. You don't need choreography or fancy moves. Sometimes it's just:
Shaking out your hands when you're anxious
Doing shoulder rolls at your desk
Taking a walk where you actually pay attention to how your feet hit the ground
Movement helps your nervous system "complete" the stress cycle. It tells your body, "Hey, the threat is over. We can relax now."
Grounding Practices These are techniques that bring you back into your body when your mind is spiraling. Examples:
Feeling your feet on the floor
Holding ice cubes in your hands
Naming 5 things you can see, 4 you can touch, 3 you can hear
It sounds simple, but these practices interrupt the anxiety loop and give your vagus nerve a chance to do its regulating thing.

The Maryland Reality Check
If you're a student or young adult in Maryland, you're probably juggling a lot, school stress, career pressure, maybe relationship stuff, plus whatever brought you to psychiatric care in the first place. The traditional model of "here's a prescription, see you in three months" doesn't always cut it.
That's why integrated care, combining medication management with somatic strategies, is becoming the standard for a lot of Maryland psych NPs and PMHNPs who actually get it. We're not replacing your meds with meditation. We're using both tools to help you feel better, faster.
As someone training in dance movement therapy while working as a psychiatric nurse practitioner, I see this integration play out constantly. A college student on Prozac for depression who also learns to recognize when they're holding tension in their jaw? They report feeling more "like themselves" than medication alone provided.
A young professional with anxiety who takes their Buspar and practices 5 minutes of grounding when they feel panic rising? They're not just managing symptoms, they're building actual resilience.
When Medication Isn't Enough
Sometimes people come to me after trying multiple medications with limited success. This is where the vagus nerve connection becomes really important. Vagus nerve stimulation (VNS) is actually FDA-approved for treatment-resistant depression, it's a device implanted near the nerve that sends regular electrical pulses.
Now, I'm not saying everyone needs a surgical intervention. But the fact that directly stimulating the vagus nerve works for severe, treatment-resistant cases tells us something crucial: vagal function matters for mental health outcomes.
If you've been on four different antidepressants and still feel stuck, it might not be about finding the "right" medication. It might be about addressing the body-level dysregulation that's keeping you in that stuck place.
What This Looks Like at Inside and Out Psychiatry
When you work with a holistic psychiatry practice, the conversation looks different. Instead of just "Are the meds working?" we're also asking:
How's your sleep?
What does your breathing pattern look like when you're stressed?
When's the last time you moved your body in a way that felt good?
How's your gut health? (Seriously, your gut and vagus nerve have a whole relationship going on.)
We're looking at the whole picture because that's what actually works. Medication management is crucial, I prescribe meds regularly, and they absolutely save lives. But they work better when your body's natural regulation systems are also online.
Your Next Move
If you're reading this and thinking, "Okay, this makes sense, but where do I start?": here's my advice:
Start small. Pick one somatic strategy and try it for a week:
Set a timer for 5-minute breathing breaks twice a day
Take a 10-minute walk where you actually notice your body moving
Try a simple grounding technique when you feel anxiety rising
Notice what changes. Not just in your symptoms, but in how you feel in your body.
And if you're in Maryland and looking for psychiatric care that takes this integrated approach seriously, check out what we do at Inside and Out Psychiatry. We combine evidence-based medication management with body-centered strategies because we know your nervous system needs both.
Your medication isn't failing you. Your body just needs to be part of the conversation.
Ready to explore what holistic psychiatry can do for you? Book a session and let's talk about the "body stuff" that might be missing from your treatment plan.

Comments